A 2025 Stanford study identified 15-PGDH as a key aging enzyme that drives osteoarthritis by breaking down cartilage and blocking natural joint repair. By inhibiting 15-PGDH, researchers successfully regenerated smooth hyaline cartilage in mice and human tissue samples, reversing cellular aging and restoring joint function without surgery. This non-surgical approach boosts prostaglandin E2 levels, reducing inflammation and promoting chondrocyte growth for lasting knee pain relief. As of January 2026, 15-PGDH inhibitors are in Phase 1 human trials for muscle recovery, with dedicated cartilage regeneration trials expected soon. This breakthrough offers real hope for reversing osteoarthritis naturally, potentially transforming treatment for millions seeking effective, minimally invasive joint repair options.
Long Version
Breakthrough in Osteoarthritis Treatment: Inhibiting the Aging Enzyme 15-PGDH for Cartilage Regeneration
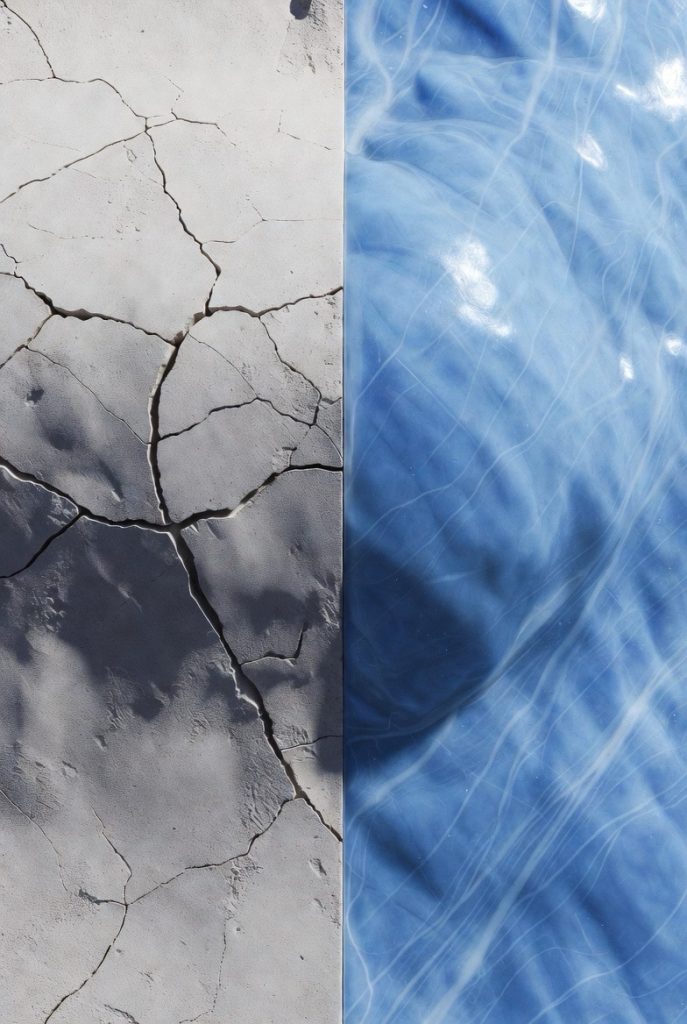
Osteoarthritis, a debilitating joint disease affecting millions worldwide, has long been considered an inevitable consequence of aging. Characterized by the breakdown of hyaline cartilage—the smooth, protective tissue covering bone ends in joints—it leads to chronic knee pain, stiffness, and reduced mobility. Traditional osteoarthritis management often relies on pain relief medications, physical therapy, or invasive procedures like knee replacement surgery. However, recent advancements in regenerative medicine are shifting the paradigm toward non-surgical arthritis treatment options that target the root causes, such as cellular aging reversal.
A pivotal 2025 Stanford study has illuminated a promising path forward by identifying 15-PGDH as a key “aging enzyme” that accelerates joint degeneration. By inhibiting this enzyme, researchers have demonstrated the potential to regenerate cartilage, offering hope for reversing osteoarthritis symptoms without the need for surgery. As of January 2026, this approach is gaining traction amid ongoing clinical trials, positioning it as a frontrunner in innovative joint repair strategies.
Understanding Osteoarthritis and the Role of Cellular Aging
Osteoarthritis treatment begins with recognizing its underlying mechanisms. Unlike rheumatoid arthritis, which involves immune system attacks, osteoarthritis stems from wear and tear, often exacerbated by age-related changes. As we grow older, chondrocytes—the cells responsible for maintaining cartilage—undergo senescence, a state where they stop dividing and contribute to inflammation and tissue breakdown. This cellular aging reversal is crucial for effective therapies.
The “aging enzyme” 15-PGDH, or 15-hydroxyprostaglandin dehydrogenase, plays a central role here. It degrades prostaglandin E2 (PGE2), a molecule essential for cell proliferation and tissue repair. Elevated levels of 15-PGDH in aged or injured joints suppress PGE2, hindering natural joint repair and promoting osteoarthritis progression. This discovery builds on prior research linking 15-PGDH to diminished regeneration in other tissues, such as muscle and bone, underscoring its status as a gerozyme—a protein that drives age-related decline.
The Landmark Stanford Osteoarthritis Study
Published in late 2025, the Stanford osteoarthritis study explored 15-PGDH inhibition as a novel cartilage regeneration technique. The team analyzed knee cartilage from aged and injured mice, as well as human tissue samples from osteoarthritis patients. They found significantly higher 15-PGDH expression in deteriorated joints, correlating with reduced hyaline cartilage regeneration.
To test their hypothesis, scientists used a small-molecule 15-PGDH inhibitor (often referred to as PGDHi or compounds like SW033291 in preclinical models). Both systemic administration (via oral or injection) and local delivery directly into the joint yielded remarkable results. In mice models of post-traumatic osteoarthritis (PTOA)—a common form triggered by injury—the treatment stimulated articular cartilage repair, reducing pain and improving joint function. The regenerated tissue closely resembled healthy hyaline cartilage, with enhanced smoothness and structural integrity. Compared to placebo, inhibiting 15-PGDH also reduced the likelihood of developing osteoarthritis after knee injury.
Extending to human applications, the study treated ex vivo human tissue samples from osteoarthritis patients. Inhibiting 15-PGDH reversed senescence markers in chondrocytes, boosting PGE2 levels and promoting cellular rejuvenation. This led to measurable hyaline cartilage regrowth, suggesting the method could enable natural joint repair in humans by reprogramming existing cells rather than introducing new ones, as in stem cell therapies. The research also builds on earlier findings that 15-PGDH inhibition can regenerate damaged muscle, nerve, bone, colon, liver, and blood cells in various models.
Mechanism: How 15-PGDH Inhibition Drives Joint Rejuvenation
At the molecular level, the 15-PGDH inhibitor acts as a prostaglandin dehydrogenase blocker, preventing PGE2 breakdown and elevating its concentrations in joint tissues. PGE2 then activates pathways that enhance chondrocyte proliferation, reduce inflammation, and facilitate extracellular matrix production—the building blocks of cartilage. This process effectively achieves senescence reversal, transforming dysfunctional cells into active contributors to tissue renewal.
Unlike traditional knee pain relief methods, such as NSAIDs or corticosteroid injections, which merely manage symptoms, this approach addresses the core issue of joint aging. It aligns with broader anti-aging enzyme strategies, where similar inhibition has shown benefits in muscle recovery, nerve repair, and even blood cell regeneration. For instance, in aged mice, 15-PGDH blockade not only regenerated cartilage but also improved overall mobility, hinting at its potential as a comprehensive arthritis cure. The treatment has also been shown to promote cartilage regeneration in old mice and prevent arthritis progression in injury models.
Current Clinical Status and Trials
As of January 2026, 15-PGDH inhibitors are in Phase 1 trials primarily for muscle recovery in conditions like sarcopenia (age-related muscle loss). An oral version of the inhibitor has been tested, demonstrating safety and activity in healthy volunteers with no significant side effects. These early results indicate increases in muscle mass and endurance, providing a foundation for expanding to joint applications.
Specific Phase 1 trials for cartilage regrowth in osteoarthritis are pending, but experts anticipate initiation soon, given the preclinical findings. Researchers hope to explore both oral formulations and anti-aging injections for joints, potentially offering a minimally invasive OA fix. This could revolutionize non-surgical joint repair, especially for knee osteoarthritis, where demand for surgery-free options is high.
Broader Landscape of Latest Treatments for Osteoarthritis in 2026
While 15-PGDH inhibition stands out, it’s part of a vibrant field of emerging arthritis advancements. For example, low-dose radiation therapy has shown promise in reducing knee pain without surgery, providing relief in up to 70% of patients with no notable side effects. This non-invasive treatment targets inflammatory and degenerative conditions in tendons and joints, offering a gentle alternative for symptom management.
Genicular artery embolization, a minimally invasive procedure, blocks abnormal blood vessels to alleviate inflammation and pain in the knee. Funded studies have demonstrated its safety and effectiveness, potentially delaying or preventing the need for knee replacement. Other regenerative approaches like viscosupplementation and mesenchymal stem cell therapies continue to evolve, with injectable biologics enhancing joint lubrication and repair.
Simple lifestyle adjustments, such as modifying walking techniques to reduce knee load, also offer accessible knee pain relief. Precision medicine, tailoring treatments based on genetic profiles, further refines these options, moving toward personalized OA reversal. Alternative therapies, including acupuncture, massage, or chiropractic care, provide additional relief for some patients, complementing medical interventions.
Seasonal variations in osteoarthritis symptoms—often worsening in colder months—highlight the need for year-round strategies, with emerging therapies like enzyme-based interventions showing consistent efficacy across demographics.
Future Implications and Considerations
The Stanford study on cartilage regrowth in mice and humans opens doors to a new era of geriatric cell rejuvenation. If Phase 1 trials for cartilage regeneration succeed, we could see regulatory approvals by the late 2020s, transforming osteoarthritis from a chronic condition to a reversible one. However, challenges remain, including ensuring long-term safety and scalability for widespread use.
Patients exploring how to regenerate knee cartilage naturally should consult healthcare providers, as self-administered remedies lack the precision of targeted inhibitors. Meanwhile, ongoing research into related gerozymes could complement 15-PGDH strategies for even more robust joint rejuvenation.
In summary, inhibiting 15-PGDH represents a groundbreaking step in osteoarthritis treatment, blending anti-aging science with practical joint repair. As trials progress, this could provide millions with a non-invasive path to restored mobility and pain-free living, redefining aging’s impact on our joints.