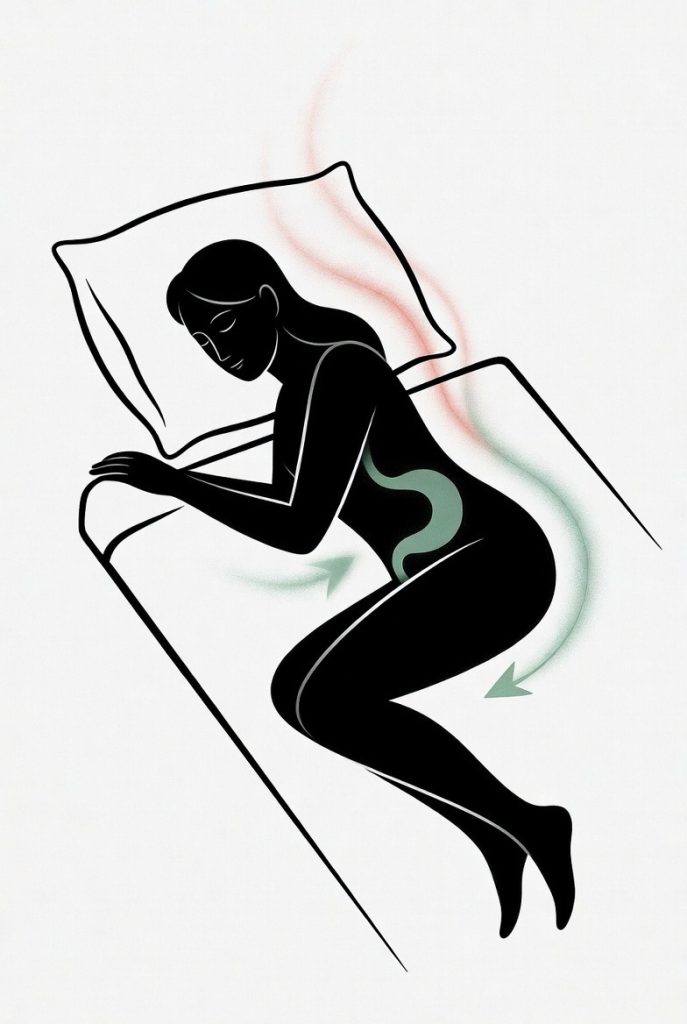
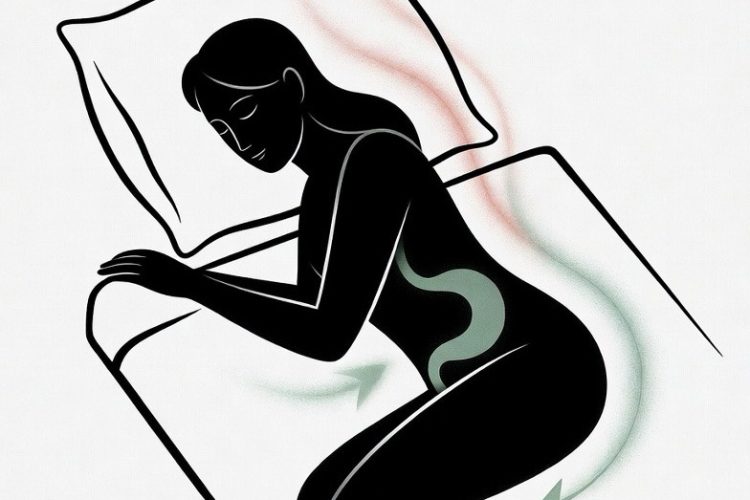
Sleeping on your left side—called the left lateral decubitus position—is widely supported by research as the best way to improve digestion and reduce acid reflux. Gravity keeps the stomach below the esophagus, helping the lower esophageal sphincter stay closed and cutting reflux episodes by up to 50%. This lowers heartburn, nocturnal GERD symptoms, and esophageal acid exposure while speeding up gastric emptying and waste transit through the colon for more regular bowel movements and less bloating. Right-side or back sleeping can worsen reflux by letting acid pool or flow upward, but left-side aligns naturally with your digestive anatomy. For better results, pair it with raising the head of your bed 6-8 inches, avoiding heavy meals before bed, and maintaining a healthy weight. This simple, non-invasive change often leads to better sleep and overall gut comfort.
Long Version
The Science of Sleeping on Your Left Side: Enhancing Digestion and Alleviating Acid Reflux
In the quest for better health, simple adjustments like changing your sleep position can yield significant benefits. Among these, adopting the left lateral decubitus (LLD) position—sleeping on your left side—stands out as a practical strategy supported by clinical data. This approach leverages gravity to optimize digestion, reduce acid reflux, and promote overall gastrointestinal comfort. Whether you’re dealing with occasional heartburn or chronic gastroesophageal reflux disease (GERD), understanding how your recumbent position influences stomach acid flow and waste transit can empower you to make informed choices for better sleep and digestive health.
The Role of Sleep Position in Digestion
Digestion doesn’t pause when you sleep; in fact, your body’s position during rest plays a crucial role in how efficiently your system processes food and eliminates waste. The LLD position aligns with the natural anatomy of your digestive tract, facilitating smoother gastric emptying and bowel movements. Gravity assists in moving contents from the stomach through the intestines, accelerating colon acceleration and enhancing waste transit.
Specifically, the ileocecal valve, located on the left side of the body, serves as the gateway between the small and large intestines. When you sleep in the LLD position, gravity promotes the seamless movement of waste into the colon, reducing the likelihood of stagnation that can lead to constipation or irregular bowel movements. This is particularly beneficial for individuals with conditions like irritable bowel syndrome (IBS), where consistent waste transit supports morning regularity and overall gut health. Additionally, this position can help minimize bloating and discomfort by encouraging the natural flow of digestive gases and fluids, contributing to a more restful night and energized morning.
By contrast, other positions may hinder this process, potentially slowing digestion and contributing to discomfort upon waking. For those with slower digestive motility, incorporating LLD can complement dietary changes, such as increasing fiber intake, to further promote efficient waste transit and colon health.
Mitigating Acid Reflux and GERD Through Strategic Positioning
Acid reflux, often manifesting as heartburn or nocturnal reflux, occurs when stomach acid backs up into the esophagus, irritating its lining and disrupting sleep. GERD, a more persistent form, amplifies these issues with frequent nocturnal GERD symptoms such as coughing, sour taste, or chest pain. The key to relief lies in maintaining the stomach below the esophagus, which the LLD position achieves naturally.
In this setup, gravity keeps the gastroesophageal junction—the point where the esophagus meets the stomach—in a favorable alignment, minimizing esophageal acid exposure. The lower esophageal sphincter (LES), a muscular ring that acts as a barrier against reflux, functions more effectively when not challenged by improper positioning. Studies using esophageal pH monitoring have shown that LLD reduces acid exposure time (AET), the percentage of time the esophagus is exposed to pH below 4, and acid clearance time (ACT), the duration needed to neutralize reflux episodes. This can cut reflux episodes by up to 50%, providing substantial relief from the burning sensation of heartburn and preventing long-term damage to the esophageal lining.
Furthermore, for pregnant individuals or those with hiatal hernias, LLD can offer additional support by reducing pressure on the LES, which may weaken under these conditions. Over time, consistent use of this position may decrease reliance on antacids or other over-the-counter remedies, fostering a more sustainable approach to managing reflux.
Evidence from Clinical Studies
A growing body of research underscores the advantages of LLD for both digestion and reflux management. Systematic reviews and meta-analyses of studies have analyzed data from randomized and nonrandomized trials, revealing that LLD significantly lowers AET and ACT compared to other positions. For instance, mean differences in AET were -2.03% versus right lateral decubitus (RLD) and -2.71% versus supine position, with similar improvements in ACT. These metrics, derived from esophageal pH monitoring, highlight reduced esophageal acid exposure and fewer reflux episodes overall.
In practical applications, experiments with participants suffering from severe nocturnal reflux have used vibrating devices to encourage LLD throughout the night, observing decreased stomach acid in the esophagus and faster clearance back to the stomach. Participants reported improved sleep quality and fewer symptoms, aligning with broader findings that LLD enhances GERD-related quality of life.
Beyond reflux, evidence links LLD to digestive efficiency. Clinical insights indicate that this position supports the natural progression of food through the intestines, promoting colon acceleration and regular bowel movements by aiding gravity-assisted waste transit. While more large-scale trials are needed, existing data from observational studies suggest it may alleviate symptoms in digestive disorders, offering a non-invasive complement to medical treatments. Emerging research also explores how LLD influences gut microbiota balance, potentially reducing inflammation and supporting immune function through better digestive flow.
Comparing Sleep Positions: LLD Versus Alternatives
Not all sleep positions are equal when it comes to gastrointestinal health. The right lateral decubitus (RLD) position, for example, positions the stomach above the esophagus, allowing gravity to exacerbate acid reflux and prolong reflux episodes. This can increase AET and ACT, worsening nocturnal GERD symptoms.
The supine position, or sleeping on your back, permits stomach acid to pool at the gastroesophageal junction, heightening the risk of nocturnal reflux and heartburn. Prone sleeping (on the stomach) adds abdominal pressure, potentially forcing acid upward and disrupting gastric emptying.
In contrast, LLD emerges as the gold standard, with studies showing no significant differences in drawbacks for most people, though some research notes potential minor effects on heart positioning that warrant further investigation. Overall, shifting to LLD from less optimal recumbent positions can markedly improve both digestion and reflux control. For side sleepers who alternate sides, prioritizing LLD for the majority of the night can still provide notable benefits, especially if combined with mindful transitions.
Practical Tips and Lifestyle Modifications
Incorporating LLD into your routine is straightforward but effective when combined with other lifestyle modifications. Start by using body pillows to maintain the position throughout the night, or consider electronic sleep positional therapy devices that gently vibrate to discourage rolling onto your back or right side.
For enhanced results, pair LLD with head elevation—raising the head of your bed by 6-8 inches to further leverage gravity against reflux. Avoid large meals close to bedtime to minimize stomach acid production, and focus on weight management, smoking cessation, and reduced alcohol intake to strengthen the LES and support overall digestion. Timing your last meal at least three hours before sleep allows for initial gastric emptying, reducing the volume of contents that could reflux.
Additionally, staying hydrated during the day but limiting fluids in the evening can prevent dilution of stomach acid, which might otherwise increase reflux risk. For those with allergies or sinus issues, LLD may also aid in drainage, indirectly supporting better breathing and sleep quality. If symptoms persist, consult a healthcare provider for personalized advice, as persistent GERD may require additional interventions like medication or esophageal pH monitoring for diagnosis.
Final Thoughts
Embracing the left lateral decubitus position offers a science-backed way to enhance digestion, accelerate waste transit through the colon, and combat acid reflux and GERD. By integrating gravity’s natural pull with your body’s anatomy, this simple change can lead to fewer reflux episodes, improved bowel movements, and better sleep quality. As research continues to affirm these benefits, LLD stands as an accessible, evidence-based tool for anyone seeking to optimize their gastrointestinal health without invasive measures. With consistent practice, it can become a habitual part of your nightly routine, contributing to long-term wellness and vitality.