Stress profoundly impacts the immune system by activating the HPA axis, releasing cortisol and catecholamines that initially prepare the body for threats but, when chronic, lead to immune suppression at the cellular level. While acute stress can temporarily enhance immune vigilance by mobilizing cells and boosting surveillance, prolonged stress disrupts mitochondrial energy production, overwhelms the endoplasmic reticulum causing proteotoxic buildup, induces lymphocyte apoptosis, and skews cytokine balance toward persistent low-grade inflammation. This dysregulation weakens defenses against infections, heightens risks for autoimmune conditions and impaired cancer surveillance, and accelerates immune aging through psychological and social stressors. Fortunately, practical steps like mindfulness practices, regular moderate exercise, anti-inflammatory nutrition, quality sleep, and strong social connections can restore balance, lower cortisol, and rebuild cellular resilience for better overall health.
Long Version
How Stress Suppresses Immune Function at the Cellular Level
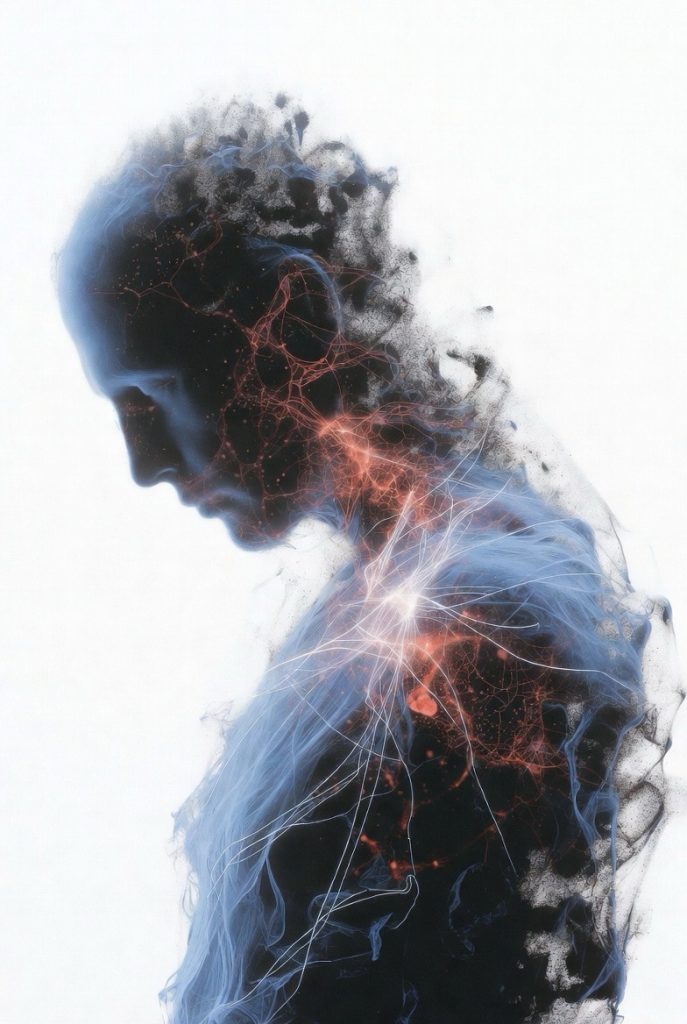
In today’s fast-paced world, stress often feels like a constant companion, subtly undermining our health in ways we might not fully appreciate. Imagine navigating a demanding day only to catch a lingering cold that refuses to fade—could your body’s defenses be faltering under pressure? The intricate link between stress and the immune system reveals how persistent tension can suppress vital protective mechanisms, particularly through subtle cellular disruptions. This comprehensive exploration unpacks how stress affects the immune system, from broad hormonal influences to precise molecular shifts, offering fresh perspectives on building resilience. Whether you’re grappling with daily pressures or seeking deeper understanding, this guide illuminates the science, highlights nuances like acute versus chronic effects, and provides practical strategies to safeguard your well-being.
We’ll navigate this topic systematically, beginning with foundational concepts and advancing to cellular intricacies, ensuring a clear path to actionable insights.
The Foundations: How Stress Interacts with the Immune System
At its essence, the connection between stress and immune system function stems from the body’s evolutionary response to threats. When stress strikes, the hypothalamic-pituitary-adrenal (HPA) axis springs into action, orchestrating the release of hormones that prepare us for immediate challenges. This neuroendocrine pathway, intertwined with the sympathetic nervous system, floods the body with cortisol and catecholamines like adrenaline, initially sharpening focus and energy.
The immune system operates through two main arms: the innate branch, which provides rapid, non-specific defense via cells like macrophages and neutrophils, and the adaptive branch, involving targeted responses from T-cells and B-cells. Stress hormones bind to receptors on these cells, modulating their activity. In balanced scenarios, this interaction maintains homeostasis, but imbalances lead to immune dysregulation stress, where defenses falter.
A key distinction emerges in how stress weakens immunity based on duration. Acute stress, such as a brief adrenaline rush during exercise, can temporarily bolster immune vigilance by redistributing cells and enhancing surveillance. However, chronic stress immune function suffers as sustained hormone exposure shifts the system toward suppression, increasing vulnerability to pathogens and delaying recovery.
Stress Hormones: Key Players in Immune Modulation
Delving deeper, stress hormones drive the effects of stress on immune system performance through direct and indirect pathways.
- Cortisol’s Multifaceted Role: As the primary glucocorticoid, cortisol regulates inflammation by suppressing pro-inflammatory signals. Yet, in prolonged stress, cells develop glucocorticoid resistance, diminishing this control and allowing unchecked inflammation. This resistance arises from downregulated receptors, perpetuating a pro-inflammatory state that exhausts immune resources.
- Catecholamines’ Influence: Adrenaline and noradrenaline activate beta-adrenergic receptors on immune cells, altering their distribution and function. Short-term, this mobilizes defenses; long-term, it impairs natural killer (NK) cell activity, crucial for viral and tumor control, potentially reducing effectiveness by significant margins.
- Cytokine Dynamics: Stress disrupts cytokine balance, elevating pro-inflammatory molecules like IL-6 and TNF-alpha while dampening anti-inflammatory ones. This skew fosters low-grade inflammation, a silent contributor to fatigue and disease susceptibility, highlighting the psychological stress immune system link where emotional strain translates to physical imbalance.
Emerging insights emphasize epigenetic modifications: chronic stress alters gene expression in immune cells, embedding long-lasting changes that favor suppression. For instance, sustained cortisol exposure can modify DNA methylation patterns, reducing the responsiveness of T-cells and B-cells over generations of cell division.
Cellular-Level Insights: Mechanisms of Suppression
The true depth of how stress suppresses immune responses unfolds at the cellular level, where stress-induced signals cascade into functional impairments.
Mitochondrial and Energy Disruptions
Immune cells demand high energy for activation and proliferation, relying on mitochondria for ATP production. Chronic stress elevates reactive oxygen species (ROS), damaging mitochondrial structures and impairing bioenergetics. In macrophages, this leads to reduced phagocytic capacity, while NK cells experience diminished cytotoxicity. The result is a fatigued immune landscape, where cells struggle to mount robust responses, exacerbating infection risks.
Endoplasmic Reticulum and Proteotoxic Stress
The endoplasmic reticulum (ER) oversees protein synthesis and folding, a process overwhelmed by stress. This triggers the unfolded protein response (UPR), aiming to restore balance, but persistent activation promotes proteotoxic stress. In T-cells, accumulated misfolded proteins activate AKT pathways, sustaining suppression and hindering proliferation. Dendritic cells, vital for antigen presentation, show impaired maturation, weakening the bridge between innate and adaptive immunity.
Macrophage Polarization and Neutrophil Impairment
Stress influences macrophage phenotypes, shifting them toward an anti-inflammatory M2 state under chronic conditions. While this curbs excessive inflammation, it hampers pathogen clearance. Neutrophils, first responders to infection, face reduced phagocytic activity and increased apoptosis, diminishing frontline defenses. These shifts illustrate cellular level stress immunity nuances, where adaptation turns maladaptive over time.
Lymphocyte Dynamics and Regulatory Shifts
T-cells and B-cells bear the brunt of suppression. Chronic stress expands regulatory T-cells (T-regs), which dampen overactive responses but can overly inhibit anti-pathogen efforts. Beta-adrenergic signaling reduces effector T-cell proliferation, while glucocorticoid pathways induce apoptosis, depleting lymphocyte pools. B-cells produce fewer antibodies, compromising humoral immunity and vaccine responses.
These mechanisms converge in immune dysregulation, where acute vs chronic stress immunity contrasts sharply: brief stress enhances innate boosts, but prolonged exposure fosters a suppressed, inflamed state prone to autoimmunity.
External Influences: Psychological, Social, and Systemic Factors
Stress doesn’t operate in isolation; psychological stress and immune system interactions amplify through broader contexts.
Mental Health Connections
Anxiety and depression heighten HPA activity, sustaining cortisol spikes that foster glucocorticoid resistance. This bidirectional loop—where immune inflammation feeds back to brain function—explains why mental strain increases pro-inflammatory cytokines, linking to conditions like autoimmune disorders.
Social Stressors and Accelerated Aging
Social stress immune aging accelerates through mechanisms like telomere shortening and immunosenescence. Loneliness or conflict expands “exhausted” T-cells, reducing naive cell diversity and impairing novel threat responses. Diverse populations may experience amplified effects due to societal pressures, underscoring the need for inclusive approaches.
Organ-Level Impacts and the Gut-Immune Axis
Beyond cells, stress affects peripheral organs. In the gut, it disrupts the microbiome-gut-brain axis, altering short-chain fatty acid production that supports immune regulation. Spleen and liver changes contribute to metabolic shifts, while lung inflammation heightens respiratory vulnerabilities. These systemic effects reinforce how stress hormones immune function ties extend body-wide.
Health Implications: From Vulnerability to Disease
The cumulative toll manifests in diverse outcomes, emphasizing the urgency of addressing stress.
- Infection Susceptibility: Suppressed NK and T-cell activity heightens risks for viral and bacterial invasions, with studies noting reduced lymphocyte counts under chronic pressure.
- Inflammatory and Autoimmune Risks: Persistent cytokine imbalances promote unnecessary inflammation, potentially exacerbating rheumatoid arthritis or multiple sclerosis.
- Cancer and Surveillance: Impaired tumor detection allows unchecked growth, as stressed systems falter in eliminating aberrant cells.
- Cardiovascular and Metabolic Ties: Inflammation contributes to atherosclerosis and insulin resistance, creating a web of interconnected health challenges.
- Mental-Physical Feedback: Immune shifts can worsen mood, perpetuating cycles that demand holistic intervention.
Balanced perspectives note that mild, managed stress may build adaptive resilience, training the immune system for future challenges without overwhelming it.
Practical Strategies: Building Immune Resilience Against Stress
Empowering yourself starts with targeted actions to counter suppression.
- Mindfulness and Relaxation Techniques: Practices like meditation lower cortisol, restoring cytokine equilibrium and enhancing vagal tone for parasympathetic dominance.
- Physical Activity: Regular moderate exercise normalizes hormone levels, boosting NK activity and countering mitochondrial fatigue.
- Nutritional Interventions: Anti-inflammatory diets rich in omega-3s, antioxidants, and fiber support gut health and buffer cellular stress.
- Sleep Optimization: Quality rest facilitates immune repair, mitigating ER stress and lymphocyte depletion.
- Social and Behavioral Support: Fostering connections reduces isolation’s toll, while therapies like cognitive behavioral approaches recalibrate HPA responses.
- Supplements with Caution: Adaptogens or vitamins may aid, but consult professionals to avoid imbalances.
Integrating these fosters a proactive stance, transforming stress from foe to manageable factor.
Conclusion: Harnessing Knowledge for Lasting Well-Being
Ultimately, understanding how stress suppresses immune function at the cellular level—from HPA-driven hormone surges to mitochondrial and ER disruptions—equips you to navigate its challenges. By appreciating the effects of stress on immune system dynamics, including acute enhancements versus chronic pitfalls, and embracing psychological, social, and lifestyle modulators, you gain tools for resilience. Prioritize balanced habits to mitigate risks, fostering a robust defense that supports overall vitality. In a world of inevitable pressures, this awareness empowers proactive choices, ensuring your immune system thrives amid life’s demands.