Colorectal cancer affects the colon or rectum and often starts as benign polyps that can become cancerous. Common symptoms include changes in bowel habits like persistent diarrhea or constipation, narrow stools, a feeling of incomplete evacuation, abdominal pain, cramping, bloating, blood in the stool (bright red or dark), unexplained weight loss, fatigue from anemia, and weakness. Symptoms vary by location—left-sided tumors cause more obvious bleeding and obstruction, while right-sided ones lead to vague fatigue and anemia. Advanced stages may bring severe pain, bowel obstruction, or signs of metastasis like jaundice, swelling, or breathing issues. Many symptoms mimic benign conditions such as hemorrhoids, IBS, Crohn’s disease, or diverticulitis, so persistent signs warrant medical attention. Risk factors include age over 50, family history, genetic mutations (e.g., Lynch syndrome), poor diet high in red/processed meats, obesity, smoking, heavy alcohol use, and diabetes. See a doctor for symptoms lasting over three weeks, especially blood in stool or rapid weight loss. Early detection through screening (starting at age 45) greatly improves outcomes—colonoscopy can remove polyps before they turn cancerous. Prevention involves a high-fiber diet, regular exercise, limited alcohol, no smoking, and routine screening. Caught early, colorectal cancer is highly treatable.
Long Version
Understanding Colorectal Cancer Symptoms: A Complete Guide
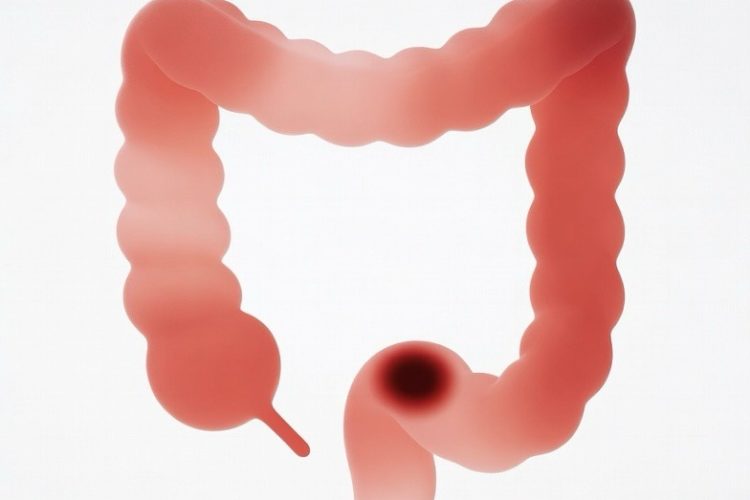
Colorectal cancer, often encompassing malignancies in both the colon and rectum, ranks among the most common forms of cancer worldwide. This colorectal malignancy, also referred to as colorectal neoplasms, arises from abnormal cell growth in the bowel, frequently starting as benign polyps that can turn cancerous over time. While the incidence of this cancer has been declining due to improved screening practices, awareness of its presenting symptoms remains crucial for early detection and better outcomes. In this article, we’ll delve deeply into the symptomatology of colorectal cancer, exploring how changes in bowel habits, abdominal discomfort, and other signs can signal this condition, while also covering risk factors, diagnosis, treatment, and prevention strategies.
Recognizing the Key Symptoms
The symptoms of colorectal cancer can be subtle at first, often mimicking less serious conditions, which is why many people delay seeking help. A hallmark change is in bowel habits, such as persistent diarrhea or constipation that lasts more than a few days. You might notice narrow stools, indicating a possible obstruction in the colon or rectum, or experience a persistent urge to have a bowel movement even after evacuation, leaving a feeling that the bowel hasn’t fully emptied. Abdominal pain, cramping, or bloating can accompany these changes, often localized but sometimes spreading throughout the belly.
Blood in the stool or rectal bleeding is another critical symptom, with the blood appearing bright red if from the lower rectum or darker if originating higher in the colon. This bleeding might not always be visible, leading to hidden blood loss that causes anemia—a low red blood cell count—resulting in fatigue, weakness, and even shortness of breath. Unexplained weight loss is common, as the body struggles with the demands of the growing tumor, and this can be exacerbated by loss of appetite or nausea.
In some cases, symptoms like dehydration may arise from severe diarrhea, while stress can amplify gastrointestinal issues, making it harder to distinguish from everyday discomfort. It’s essential to monitor these signs closely, as early-stage colorectal cancer might present with minimal symptomatology, but ignoring them could allow the disease to progress. Additional indicators can include gas pains, a sensation of fullness, or changes in stool consistency that persist despite dietary adjustments.
How Symptoms Vary by Location and Stage
The location of the cancer within the colorectal system influences the symptoms experienced. For instance, left-sided tumors in the descending colon or rectum often cause more noticeable changes, such as narrow stools, rectal bleeding, or a sense of incomplete bowel evacuation due to the narrower passage. In contrast, right-sided cancers might lead to vaguer symptoms like abdominal pain, fatigue from anemia, or unexplained weight loss, as they allow for more space before causing obstruction.
As the cancer advances through its stages—from localized polyps to invasive tumors and eventual metastasis—the symptoms intensify. In advanced stages, you may encounter severe cramping, persistent abdominal pain, or bowel obstruction, where stool passage becomes impossible. If metastasis occurs, spreading to organs like the liver or lungs, additional signs emerge: jaundice (yellowing of the skin and eyes) from liver involvement, swelling in the abdomen or legs, trouble breathing, bone pain, or even fever and itching. These metastatic symptoms underscore the importance of catching the disease early, before it reaches such a critical point. Monitoring for progression involves noting any escalation in symptom severity or the appearance of new issues, such as persistent vomiting or noticeable lumps in the abdomen.
Conditions That Mimic Colorectal Cancer Symptoms
Not every instance of abdominal pain or change in stool signals cancer; many symptoms overlap with benign issues. Hemorrhoids, for example, can cause rectal bleeding and discomfort, while irritable bowel syndrome (IBS) often presents with cramping, bloating, diarrhea, or constipation. Inflammatory conditions like Crohn’s disease or ulcerative colitis—characterized by ulcers and chronic inflammation—may lead to similar bowel habit changes, blood in the stool, and fatigue. Even infections, dietary issues, or stress-related gastrointestinal upset can mimic these signs, highlighting why professional evaluation is key to ruling out colorectal malignancy. Diverticulitis, another common condition, can cause pain and changes in bowel patterns, often accompanied by fever, further complicating self-diagnosis.
Risk Factors: Who Is Most Susceptible?
Understanding risk factors can help identify those who should be vigilant about symptoms. Age is a primary factor, with most cases occurring after 50, though incidence is rising in younger adults. Family history plays a significant role; if close relatives have had colorectal cancer or polyps, your risk increases. Genetic mutations and variants, such as those in Lynch syndrome or familial adenomatous polyposis, account for about 5-10% of cases, often leading to hereditary colorectal neoplasms.
Lifestyle elements also contribute: poor nutritional habits, including a diet high in red and processed meats with low fiber, elevate risk, as does obesity, physical inactivity, smoking, and heavy alcohol use. Conditions like diabetes, prior radiation therapy, or inflammatory bowel diseases further heighten susceptibility. Racial disparities exist, with higher rates among Black individuals in the U.S. Environmental factors, such as exposure to certain chemicals or a sedentary lifestyle, can compound these risks, emphasizing the need for holistic health management.
When to Consult a Healthcare Professional
If you experience any persistent symptoms—like blood in the stool, unexplained weight loss, or changes in bowel habits lasting three weeks or more—see a doctor promptly. Don’t hesitate due to embarrassment; a gastroenterologist can perform a thorough evaluation, starting with a physical exam, blood tests for anemia, or stool samples to detect hidden blood. Urgent attention is needed for severe signs like non-stop rectal bleeding or bloody diarrhea, which warrant emergency care. Additionally, if symptoms are accompanied by fever, severe pain, or rapid weight loss, immediate medical intervention is crucial to prevent complications.
Diagnosis: Uncovering the Cause
Diagnosis typically begins with screening tests, even before symptoms appear, such as colonoscopies to visualize and remove polyps or stool-based tests like FIT or DNA analysis. If symptoms are present, imaging like CT scans, X-rays, or virtual colonoscopies may follow, alongside biopsies to confirm cancer and determine its stage. Staging assesses how far the cancer has spread, from early localized stages to advanced metastasis, guiding treatment. Blood tests for tumor markers, like CEA, can also aid in monitoring, while endoscopic ultrasound provides detailed views of rectal tumors.
Treatment Options for Colorectal Cancer
Treatment varies by stage but often includes surgery to remove the tumor, such as colectomy or minimally invasive procedures. For advanced cases, chemotherapy, radiation therapy, targeted drugs, or immunotherapy may be employed to shrink tumors or manage metastasis. In some instances, procedures like colostomy or ileostomy are necessary. Palliative care focuses on symptom relief, ensuring quality of life. Emerging treatments, such as precision medicine tailored to genetic profiles, offer hope for more effective, personalized approaches with fewer side effects.
Prevention: Steps to Reduce Your Risk
Prevention centers on lifestyle and screening. Adopt healthy nutritional habits rich in fruits, vegetables, and whole grains to boost fiber intake, while limiting alcohol and quitting smoking. Regular exercise and maintaining a healthy weight are vital. Screening starting at age 45 (or earlier with risk factors like family history) can detect polyps before they become cancerous, dramatically lowering incidence. For high-risk individuals with genetic mutations, preventive medications like aspirin may be considered after consulting a doctor. Vaccinations against related infections, like HPV for certain anal cancers, and managing chronic conditions can further mitigate risks.
By staying informed about these symptoms and acting swiftly, you can significantly improve outcomes. Colorectal cancer is highly treatable when caught early, making awareness your strongest ally in safeguarding health. Regular check-ups and open discussions with healthcare providers empower individuals to take proactive steps toward prevention and early intervention.