Rising allergies like food allergies, asthma, and eczema are linked to poor gut health caused by pesticide exposure. Pesticides such as glyphosate disrupt the gut microbiome, killing beneficial bacteria (Lactobacillus, Bifidobacterium) and reducing microbial diversity. This dysbiosis weakens the gut barrier, triggers chronic inflammation, and impairs immune tolerance, making the body overreact to harmless allergens through IgE, histamine, and inflammatory cytokines. Short-chain fatty acids that normally calm the immune system drop, raising risk of allergic diseases and even IBD. Chronic low-dose exposure from food and environment, combined with air pollution, worsens the problem. Choosing organic produce, eating prebiotic-rich foods, and adding probiotics can help restore balance and lower allergy risk. Reducing pesticide exposure protects gut health and strengthens immunity.
Long Version
The Intricate Connection Between Pesticides, Gut Health, and Allergies
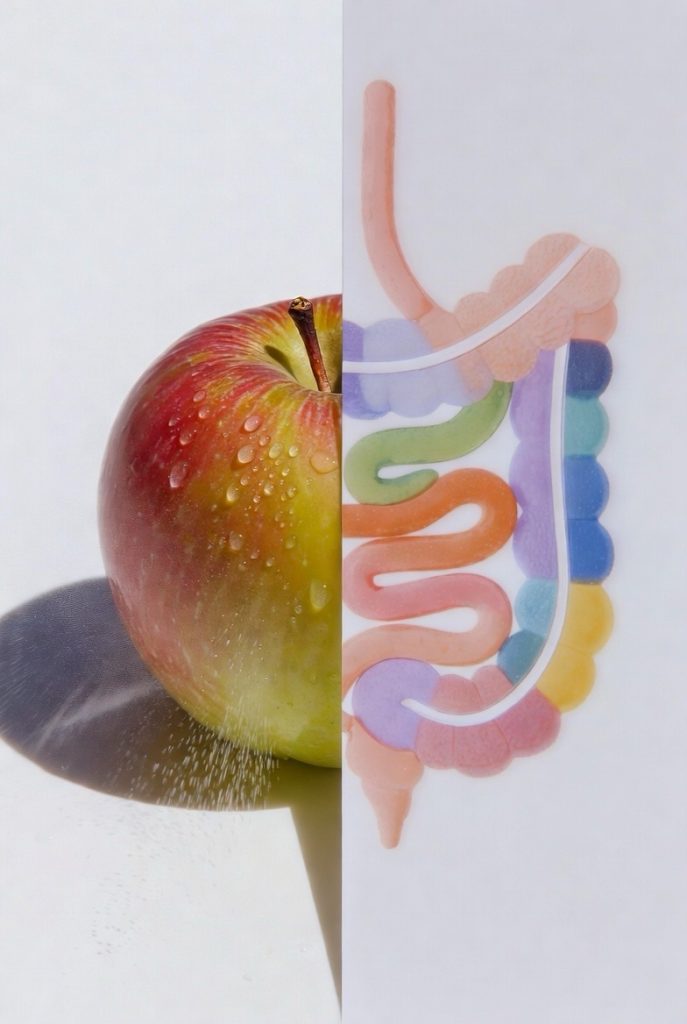
In an era where allergic diseases are on the rise, affecting millions worldwide, understanding the interplay between environmental factors and human physiology has never been more critical. Allergies, encompassing conditions like food allergies, allergic rhinitis, allergic asthma, and atopic dermatitis, often manifest as hypersensitivity reactions triggered by common allergens such as pollen, pet hair, dust, or food. These responses involve the immune system overreacting, with key players including immunoglobulin E (IgE), cytokines like IL-4, IL-5, IL-9, and IL-13, histamine, prostaglandins, and leukotrienes. Cellular components such as T-cells, B-cells, eosinophils, mast cells, and basophils drive both innate responses and acquired responses, potentially leading to severe outcomes like anaphylactic shock. Emerging research points to a pivotal role for gut health in modulating these allergic conditions, with disruptions in the gut microbiota—known as dysbiosis—linked to increased disease susceptibility. Among the environmental triggers implicated, pesticides stand out as significant contributors, altering the microbiome and fostering inflammation that heightens immune health vulnerabilities.
The Role of the Gut Microbiome in Health
The gut microbiome, a complex ecosystem of trillions of microorganisms including gut microbiota and intestinal microbiota, is essential for host immunity and overall well-being. This microbial diversity supports microbiota composition and metabolism, aiding in detoxification, processing nutrients, and maintaining biodiversity. Beneficial bacteria, such as those in probiotics like Lactobacillus, contribute to microbiota metabolism and produce short-chain fatty acids crucial for epithelial barrier integrity and immune homeostasis. Disruptions here can lead to microbiome dysbiosis, affecting not only the gut but also distant sites through bidirectional communication, including the skin microbiota and airway microbiota. The gut-brain axis further illustrates this interconnectedness, influencing neurodevelopment, neuroplasticity, and even neurodegenerative diseases. When environmental contaminants interfere, they can initiate a cascade of changes, resulting in indirect effects on functionality and metabolism, ultimately compromising host-microbe interactions and immune tolerance.
Pesticides as Environmental Contaminants
Pesticides, as a class of synthetic chemicals and environmental chemicals, represent a major source of dietary exposure and environmental contaminants. Common examples include glyphosate, phthalates, and dichlorophenols, often found alongside other pollutants like diesel exhaust and traffic-related air pollution. These xenobiotics enter the body through food, water, and air, accumulating in tissues and exerting effects on the exposome—the totality of environmental interactions over a lifetime. Studies have shown that chronic low-level exposure to these substances can profoundly impact gut microbes, altering human gut bacteria growth patterns and leading to gut microbiome alterations. For instance, glyphosate, a widely used herbicide, inhibits the shikimate pathway in bacteria, similar to its action in plants, depleting beneficial taxa and enriching opportunistic ones. This disruption extends to bacterial groups and fungal groups, reducing microbial diversity and promoting dysbiosis.
Mechanisms of Pesticide-Induced Gut Disruption
The mechanisms by which pesticides undermine gut health are multifaceted. Glyphosate, for example, has been found to affect over half of the core human gut microbiome species, leading to microbiome dysbiosis by interfering with essential biochemical pathways. This results in reduced production of short-chain fatty acids like butyrate, acetate, and propionate, which are vital for maintaining the epithelial barrier and regulating inflammation. Such alterations can exacerbate conditions like inflammatory bowel disease (IBD), including ulcerative colitis (UC) and Crohn’s disease (CD), which share inflammatory pathways with atopies and allergic skin disease. Pesticides also influence polyamine production and oxidative stress, further disturbing immune homeostasis and host immunity. In animal models, exposure to these environmental triggers has been linked to shifts in microbiota composition, increasing susceptibility to allergic diseases by impairing the gut’s role in immune tolerance.
Linking Gut Dysbiosis to Allergic Conditions
Connecting these dots reveals how pesticide-induced gut dysbiosis contributes to allergic conditions. A disrupted microbiome can weaken the epithelial barrier, allowing allergens to penetrate and trigger exaggerated immune responses, involving cytokines and leading to chronic inflammation. This is evident in the rising prevalence of food allergies and allergic asthma, where gut microbiome alterations foster an environment conducive to hypersensitivity reactions. Moreover, the gut-brain axis amplifies these effects, potentially linking early pesticide exposure to neurodevelopmental issues and altered neuroplasticity, while long-term impacts may include neurodegenerative diseases. Human studies corroborate these findings, showing that pesticide residues in food correlate with changes in gut microbes that mirror those in allergic individuals. For example, exposure to glyphosate has been associated with reduced levels of beneficial bacteria like Bifidobacterium and Lactobacillus, which are key for maintaining immune balance and preventing atopies.
Broader Environmental Influences and Risks
Broader environmental factors compound these risks. Air pollution and synthetic chemicals interact with pesticides, amplifying their effects on the microbiome and increasing disease susceptibility. Agricultural practices, including the use of pesticides on crops, affect not only human health but also the soil microbiome, which influences food quality through organic farming alternatives that preserve bacterial and fungal groups. While some critiques argue that direct causation between pesticides and allergies remains debated, requiring more epidemiological data, the converging evidence from animal and human studies substantiates a strong associative link. Notably, not all exposures lead to immediate allergic reactions, but chronic low-dose interactions appear to erode immune health over time.
Strategies for Mitigation and Protection
Mitigating these risks involves reducing dietary exposure through choices like organic produce, which minimizes pesticide residues and supports microbial diversity. Incorporating probiotics and prebiotics can help restore gut balance, potentially alleviating symptoms of allergic diseases and IBD. Public health strategies should prioritize monitoring the exposome and advocating for safer agricultural practices to protect host-microbe interactions.
Conclusion
In summary, the connection between pesticides, gut health, and allergies underscores a critical public health issue. By disrupting the microbiome and fostering inflammation, these environmental contaminants heighten vulnerability to a spectrum of allergic conditions and related disorders. Ongoing research will refine our understanding, but current evidence calls for proactive measures to safeguard immune health in an increasingly polluted world.